Out-of-Pocket Amounts Announced for 2025
The Department of Health and Human Services (HHS) recently announced the 2025 Benefit Parameters, outlining the maximum out-of-pocket (OOP) limits applicable to non-grandfathered plans for plan years beginning in 2025. Each year, these OOP maximums are adjusted for inflation. In 2023, HHS pledged to release the updated amounts “by January of the year preceding the applicable benefit year” and they have indeed stuck to that promise.
Under the Affordable Care Act (ACA), non-grandfathered health plans are required to comply with an overall annual limit on out-of-pocket expenses for essential health benefits, regardless of whether the plan is self-funded or fully insured. The current limits applicable to 2024 plan years are $9,450 for self-only coverage and $18,900 for family coverage. The 2025 limits will be lowered to $9,200 for self-only coverage and $18,400 for family coverage, respectively.
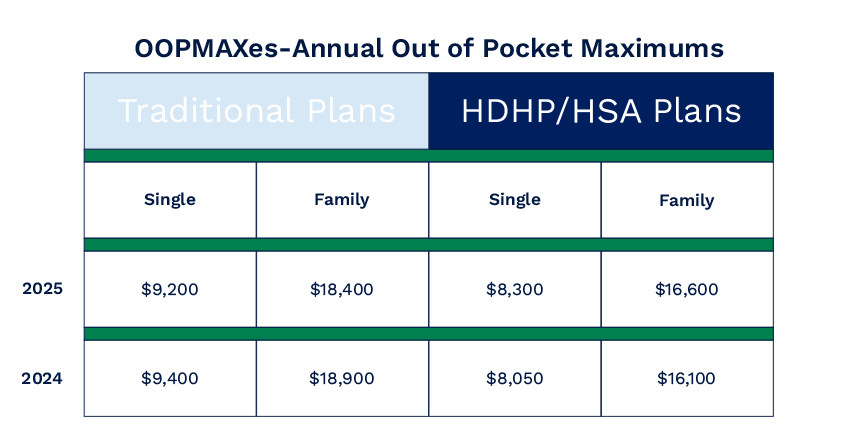
Here's a summary of the amounts for traditional plans for the 2024 / 2025 plan years for reference :
High-deductible health plans (HDHPs) with Health Savings Accounts (HSAs) feature different limits than traditional plans, including OOP maxes, along with deductible and contribution limits. Update: The 2025 HDHP/HSA limits were released by the IRS on May 9, 2024 via Rev. Proc. 2024-25. Historically these limits are released in May of each year. For 2025, the maximum out-of-pocket amount for self-only coverage is $8,300 and $16,600 for family coverage, up from $8,050 and $16,100, respectively in 2024.
Although, it should be noted that if your plans offer both traditional and HDHP/HSA plans (that are not grandfathered), your plans are subject to both sets of requirements and you must ensure compliance with the lowest applicable out-of-pocket maximum. Plus, the ACA requires that a per person (individualized/embedded) out-of-pocket maximum doesn't exceed the ACA limit, even if you are in the larger (family) tier. This assists single family members in accessing benefits sooner without having to hit the full amount for the family tier.
Additional Links:
- 2025 HDHP/HSA Limits: Rev. Proc. 2024-25
- CMS Memo
Featured News & Insights

The Medical/Rx market is facing trend factors that are reaching a 30-year high. Unfortunately, we expect these higher trend factors to continue. One of the most common concerns we hear from the...

For many HR teams and brokers, open enrollment can feel like the finish line. Months of planning, communication, and technology setup finally come together in a few fast-moving weeks. When the last...

AssuredPartners has long been committed to providing you and your teams with highly valuable content packed with deep industry expertise and innovative risk management solutions. As a valued member...